How to Handle Confusing Cost Scoring in Your MIPS Preview
By: Heather Miller | July 24th, 2023

The Centers for Medicare & Medicaid Services recently opened the MIPS 2022 Final Score preview. And already it has led to some confusion.
Some providers and practices have indicated CMS has inaccurately calculated their scores in the Cost category, resulting in a lower overall score.
This is the first time Cost data has been made available since 2019. In the previous three years, the Cost category has been re-weighted by CMS due to the Covid pandemic. Keep in mind, this is not the final score, and there is no information on payment adjustments during this preview period. Final scores and adjustments are set to be released in August, and the targeted review period will begin.
For now, all providers and practices that reported MIPS for 2022 should log in to preview their scores and confirm whether they were scored on any of the Cost measures available.
As you preview your Cost scores, refer to this Q&A to help you understand the results and inform your decision on any potential response to CMS.
Why don’t I see any Cost measure information?
Only clinicians, groups, and virtual groups who could be scored on at least one measure will see cost measure information in performance feedback.
If you don’t see any cost measure details and see a score of “N/A,” then your group didn’t meet the case minimum for any cost measures and the weight for this performance category was reallocated to another category.
Clinicians, groups, and virtual groups who were approved for re-weighting in this performance category can still access measure-level and patient-level feedback if they met the case minimum for at least one cost measure.
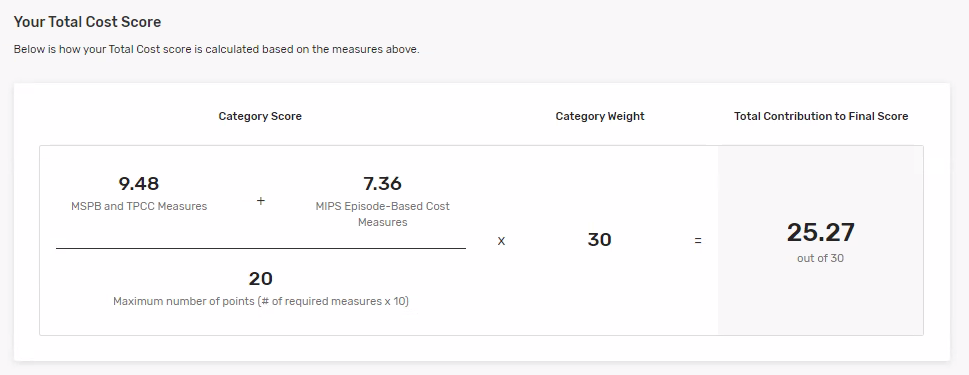
How is the Cost category score determined?
There’s a graphic at the bottom of the Cost page showing how CMS arrived at the points contributing to your final score.
- CMS will sum the points earned for each of the Cost measures you could be scored on and divide that by the maximum number of points available (10 x the number of measures you could be scored on).
- CMS will then multiply that by 30% performance category weight.
In the example below, the organization could be scored on two of the Cost measures available for scoring in the 2022 performance period.
Where can I find more information about Cost measures?
CMS will release patient-level Cost measure reports with final performance feedback in August. These reports will include every cost measure on which you could be scored.
What should I do if my practice has been scored on the diabetic measure but we do not manage chronic diabetes?
If you see a score on the Diabetes Cost Measure in your score preview report and you are in a practice that does not prescribe the medications listed in the Service_Assignment_D tab of the Diabetes measure codes list, submit a complaint to the QPP Service Center. Let them know that managing diabetes is not in your scope-of-practice and you were inappropriately attributed this measure.
Why is my score for the Cataract Episode measure so low? How is it scored?
Calculating scores for the episode-based measure is complex. Reading through the specifications and understanding how the costs are determined takes time. Without having any of the data files at this time, it will be difficult to confirm accuracy until the provider/practice can view this data. CMS will release these in August along with final scores.
In the meantime, providers and/or practices can learn more about the measure and join in conversations within society forums to stay in the know on efforts being made to request further explanation from CMS. A good starting point is reviewing this research article about how the measure was developed and evaluated.
How can I contact the QPP Service Center if I have questions about my MIPS score preview?
- Email qpp@cms.hhs.gov.
- Create a Quality Payment Program Service Center ticket online.
- Call the QPP Service Center 1-866-288-8292, 8 a.m.-8 p.m. ET Monday to Friday.
Source
The Centers for Medicare & Medicaid Services Quality Payment Program MIPS Final Score Preview Fact Sheet
HERE ARE SOME RELATED ARTICLES YOU MAY FIND INTERESTING
Ophthalmology | Compliance | CMS | Coding | Clinical Efficiency
A Step-by-Step Guide to Preparing Your Ophthalmology Practice for the New CMS Audits
By: Courtney Tesvich | November 21st, 2025
Practice Management | EHR | Billing | Revenue Cycle Management
Claims Scrubbing: Reduce Denials and Maximize Revenue in 2026
By: Nextech | February 24th, 2026