Interoperability and the MIPS Final Rule Changes for 2023
By: Lia (Parisyan) Schmidt | December 6th, 2022

Take a look at key MIPs changes in 2023 for interoperability.
To ensure your practice is ready, Nextech Senior Professional Services Consultants Kristi Brantley and Heather Miller share the changes to interoperability.
Interoperability
CMS is making several changes to the Promoting Interoperability category. To stay certified, an EHR must meet the conditions of the 2015 Cures Edition Update, which takes effect in 2023. As a result, you must be using an EHR that meets these criteria for your 90-day Promoting Interoperability performance period in 2023.
- Reporting period - Any consecutive 90 days
- Reporting requirements - Four reporting objectives
Benchmarking
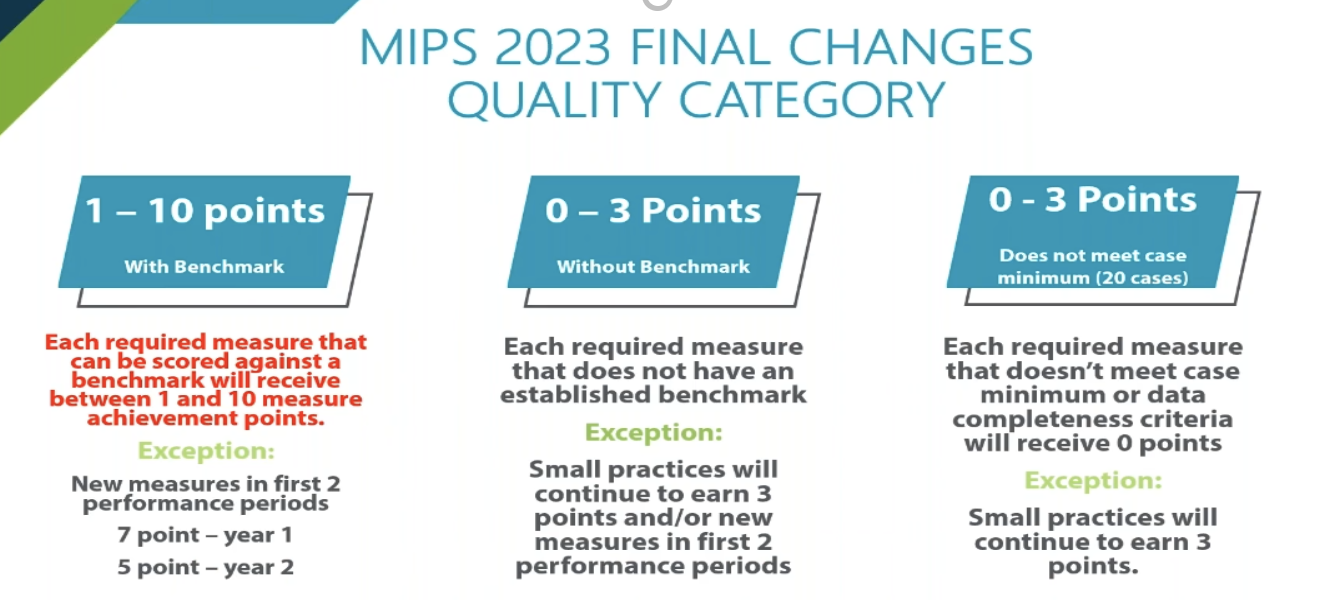
With benchmarking, each required measure that can be scored against the benchmark will receive between one and ten measure achievement points. In the past, it’s been three to ten points. So, in other words, you could get one point on a measure with a benchmark depending on what you’re scoring on that measure.
New measures in the first two performance periods; in the first year of the measure, you’re looking at a seven to ten benchmark, and in the second year, you are looking at a five-to-ten-point scale.
Each required measure that doesn’t have an established benchmark will be zero to three points except for small practices that will continue to earn three points or new measures in the first two performance periods.
Additionally, each required measure that doesn’t meet the 20-case minimum or data completeness criteria will receive zero points. However, small practices will continue to earn three points.
💡 Expert tip: Check your eligibility and special statuses to see if you are considered a small practice. 15 physicians or fewer is considered a small practice.
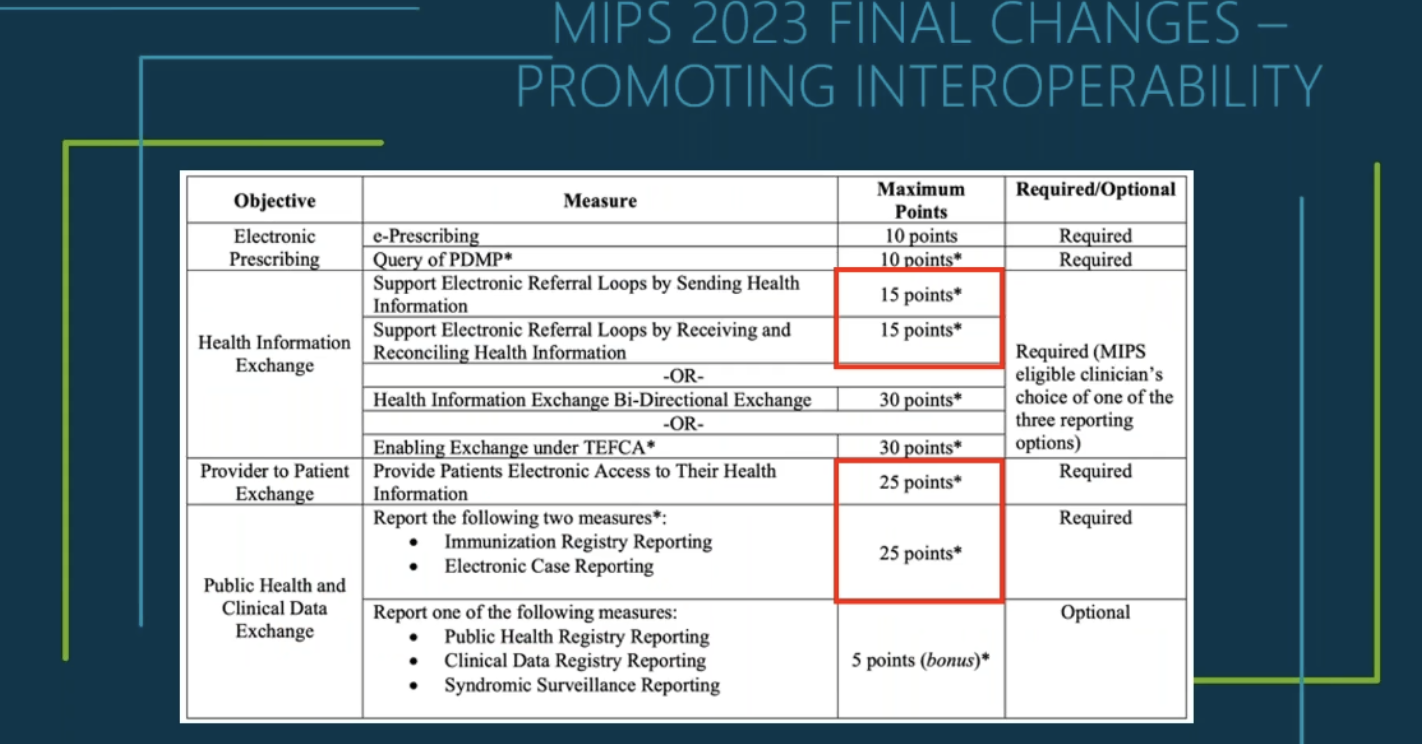
Promoting Interoperability (PI) category major changes:
- There is still an automatic reweight applied for small practices.
- Provider provides patient exchange decreased from 40 points to 25.
- Public health and clinical data exchange increased from 10 points to 25.
- Query of PDMP is now 10 points and it is required – Confirm State PDMP requirements
- 5 bonus points is available for additional data exchange for : Clinical Data Registry, Public Health and/or Syndromic Surveillance
The Trusted Exchange Framework and Common Agreement (TEFCA's) goal is to establish a universal policy for nationwide interoperability, simplify connectivity for organizations to securely exchange information to improve patient care, enhance the population's welfare, and generate health and care value. It also enables individuals to gather their healthcare information.
Prescription Drug Monitoring Program (PDMP)
The PDMP follows state jurisdiction and may have mandatory requirements outside the minimum. So, MIPS requires you to use a prescription drug monitoring program, but your state may also have requirements to follow.
There are three finalized MIPS exclusions:
- You cannot electronically prescribe Schedule II opioids and Schedule III and IV drugs under applicable law during the performance period.
- You write fewer than 100 permissible prescriptions during the 90-day performance period.
- New for 2023 ONLY: Querying a PDMP would impose an excessive workflow of cost burden before your selected 90-day performance period. You can take this exclusion only in 2023.
💡 Expert tip: The PDMP query can be completed through an integrated solution or directly through the state site. So, if you have an ePrescribing software that has PDMP built in, you can do it there or go out to the state site and do it that way. Visit the EPCS Gold website for more resources on state requirements.
Electronic Case Reporting
There are three finalized MIPS exclusions if the MIPS-eligible clinician:
- Does not treat or diagnose any reportable diseases for which their jurisdiction's reportable disease system collects data during the performance period.
- Operates in a jurisdiction where no public health agency can receive electronic case reporting data in the specific standards required to meet the CEHRT definition at the start of the performance period.
- Operates in a jurisdiction where no public health agency has declared readiness to receive electronic case reporting data as of six months before the start of the performance period.
Watch the MIPS Final Rule 2023 Webinar
To learn more about these topics, explore your submission options, refine your quality measure selection, and discover reasons why to stay in MIPS, watch the on-demand webinar specific to your specialty: Dermatology | Ophthalmology | Orthopedics | Plastic Surgery
HERE ARE SOME RELATED ARTICLES YOU MAY FIND INTERESTING
Ophthalmology | Compliance | CMS | Coding | Clinical Efficiency
A Step-by-Step Guide to Preparing Your Ophthalmology Practice for the New CMS Audits
By: Courtney Tesvich | November 21st, 2025
Ophthalmology | AAO | Technology & Innovation | AI
Bringing the Future into Focus at AAO 2025
By: Amanda Wratchford | October 27th, 2025
How to Bill Bilateral Procedures in Ophthalmology: Modifier 50 Explained
By: Nextech | October 17th, 2025