Latest Articles
The latest news and information regarding electronic medical records, practice management software, HIPAA, and security from Nextech.

By:
Nextech
January 2nd, 2015
October 1, 2015. Why is this date extremely vital for your specialty-specific medical practice? One word: ICD-10-CM. ICD-10-CM has to be fully implemented in your practice by this date – or else all of your insurance claims for clinical treatment after this deadline will be denied. Therefore, some major preparations are necessary to continue receiving insurance reimbursements for your medical services. To assist you in your ICD-10 journey, we would like to give you 6 tips on how to execute a smooth and successful transition with the least number of road bumps along the way. Naturally, the earlier you and your personnel begin to actively get ready, the easier it will be to monitor your revenue cycle after October 1, 2015. Therefore, don’t procrastinate on ICD-10 until the last minute.

Clinical Efficiency | Healthcare Technology
By:
Nextech
December 29th, 2014
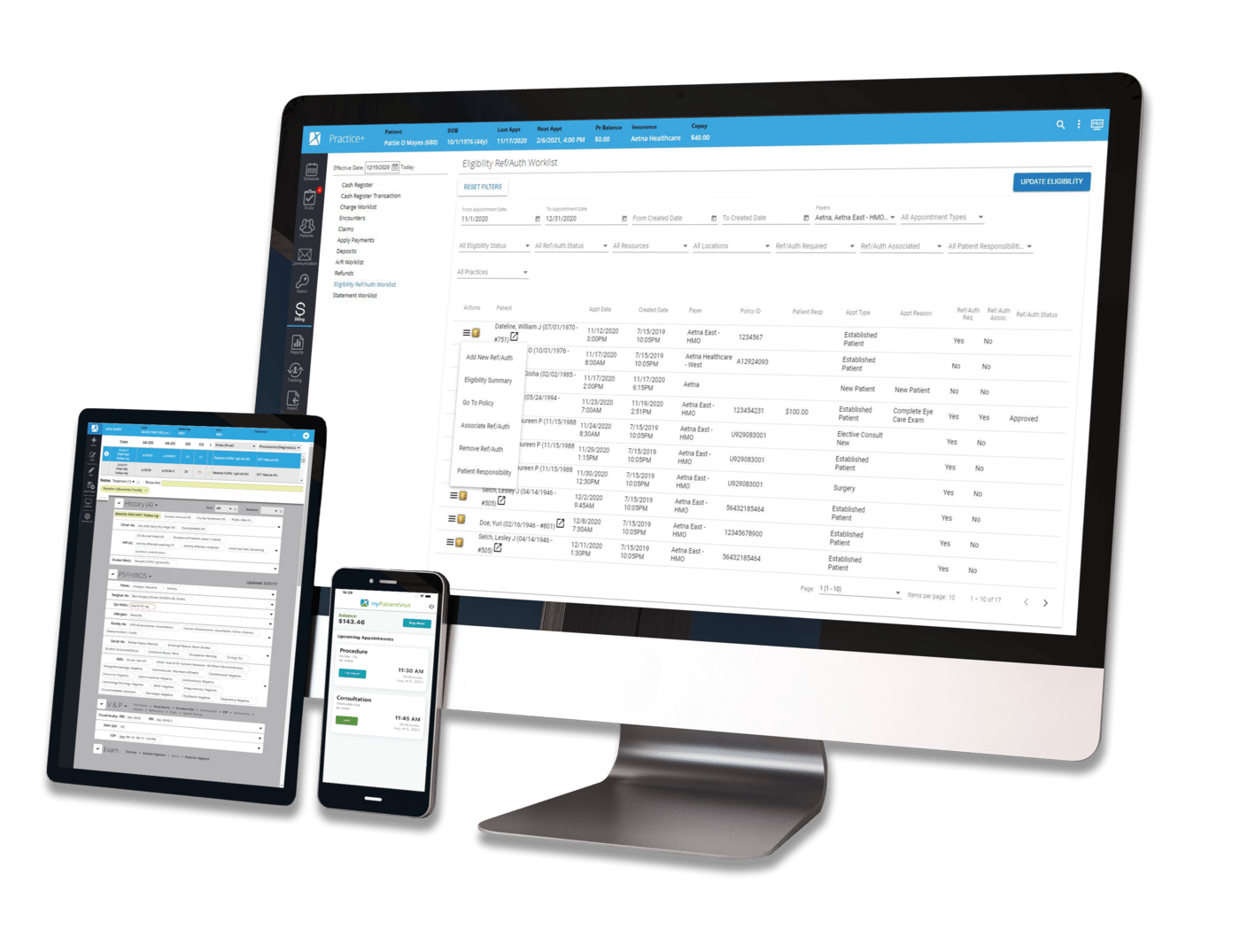
As patients assume increasing responsibility for personal healthcare costs, determining eligibility has become essential to patient satisfaction—and to protecting the practice’s revenue cycle. When patients who are accustomed to incurring only minor co-pays receive bills that are far greater than expected, those who can’t pay or resist payment can represent very difficult collections. This can be especially problematic for specialty practices that have different co-pays from primary care providers or services that may require referral or preauthorization for coverage.

By:
Nextech
December 12th, 2014
The disruptive nature of the transition to ICD-10 poses serious questions for specialty practices; and while we’ve worked to address many questions in this blog, including how ICD-10 works, key differences between it and ICD-9, steps for preparing your clinical functions and readying your overall practice, and how an EMR can minimize ICD-10 disruption, there still is one lingering question: Do we really need it?

Regulatory & Compliance | Healthcare Technology
By:
Nextech
December 11th, 2014
Have you implemented certified EMR/EHR technology in your specialty practice? The 2009 American Recovery and Reinvestment Act (ARRA) required reimbursement penalties for all Medicare eligible healthcare providers who do not comply with Meaningful Use.

By:
Nextech
December 9th, 2014
Nextech will be hosting its first annual user conference, EDGE (Educate, Discover, Generate, Exchange), Wednesday, February 25, 2015 to Friday, February 27, 2015 at Walt Disney World’s Swan and Dolphin Resort in Lake Buena Vista, Florida. Warning: If you are looking for a boring, sleep-inducing conference, EDGE isn’t for you. If you want a dynamic, hands-on training and networking experience on the very latest in effective practice solutions, you should definitely plan to attend this conference. This will be a memorable experience with things to do for the whole family.

Regulatory & Compliance | Healthcare Technology
By:
Nextech
November 24th, 2014
Most specialty practices set aside ample time for software systems training when implementing new technologies. It’s typically all-hands-on-deck for vendor training during EMR implementation, and many host topic-specific training sessions to support meeting Stage 2 requirements for practices that pursue meaningful use. In addition, most practices that bill any insurance companies are currently focused on training in preparation for the ICD-10 transition. But what about the long stretches in between milestones?

By:
Nextech
November 19th, 2014
ICD stands for International Classification of Diseases. This international standard is used to document all different types of diseases and other health-related conditions in many official medical records. Most member states of the World Health Organization (WHO) started using ICD-10 (the most up-to-date version) since 1994. The United States is one of the few WHO members that still uses ICD-9 and has not yet transitioned to ICD-10.

Security & Data Management | Healthcare Technology
By:
Nextech
November 17th, 2014
Has a virus ever hit your computer networks or EMR software? How about a hard-drive failure, data leak, or someone with unauthorized access to your software (i.e. a hacker)? If you have experienced one or more of these IT issues, then you’re probably no stranger to the disastrous consequences it can have for your practice.