
The Department of Central Management Services’s (CMS) Quality Payment Program (QPP) aims to improve the quality of American healthcare and reduce administrative burden on clinicians by collecting data on patients, interventions, and outcomes.
The hard part is identifying the right data and gathering enough of it to extract valuable insights.
Enter eCQMs: electronic clinical quality measures. This structured data is extracted directly from the records of reporting practices, making it more accurate and easier to collect than other kinds of data.
What Are eCQMs? And How Are They Different?
CQMs are data measures healthcare practices report to CMS. Traditionally, this data is collected and entered by staff at the practice. eCQMs are automatically extracted from the electronic health record (EHR) and submitted electronically, with no manual intervention required.
If you’ve been reporting quality measures to CMS, you’re probably familiar with MIPS CQMs and Medicare CQMs. While your practice can choose between traditional and eCQMs for now, there is a plan to phase out manual reporting.
MIPS, MIPS Value Pathways, and MSSP ACOs all require practices to report at least some quality measures electronically.
Eventually, all data for all CMS Quality Payment Programs (QPP) will be electronically collected. It’s difficult to say when the shift will officially take place; as of 2025, there are only 47 measures available to report as eCQMs.
As their role in reporting grows, eCQMs might feel like another complicated mandate to figure out, but they’re actually intended to make reporting easier.
CQM vs. eCQM
|
Traditional CQM |
eCQM |
|
Data is manually entered by staff |
Data is automatically extracted from the EHR |
|
Reports are manually uploaded to CMS |
Reports are electronically submitted in near real- time |
|
Reports are vulnerable to human error |
Reports are more likely to be accurate |
Do Specialty Practices Need to Report eCQMs?
While not every measure can be reported as an eCQM, it’s advisable to start electronically reporting what you can. CMS has made it clear eCQMs are soon to be the standard for CMS quality reporting.
Some eCQMs apply specifically to specialty practices, such as a visual acuity measure following cataract surgery. Others, like “closing the referral loop: receipt of specialist report” apply across specialties.
How to Succeed with eCQMs in 2025
The performance period for all CMS QPP programs is the calendar year, from January 1 through December 31. Each year, quality measures in each program change, so it’s important to keep the members of your practice up to date.
Once you’ve decided which QPP your practice will participate in and which quality measures you will report, conduct internal audits to find gaps in your reporting. Use the dashboards and data analytics in your EHR to track your performance against benchmarks.
Set Up Your EHR for eCQM Success
Unlike traditional CQMs, no one on your staff manually enters eCQM data. It flows directly from your EHR into a report.
While this means less repetitive manual work, it also means your staff must understand the EHR’s workflow. This workflow is how the data gets from the patient chart to the correct place in the performance report.
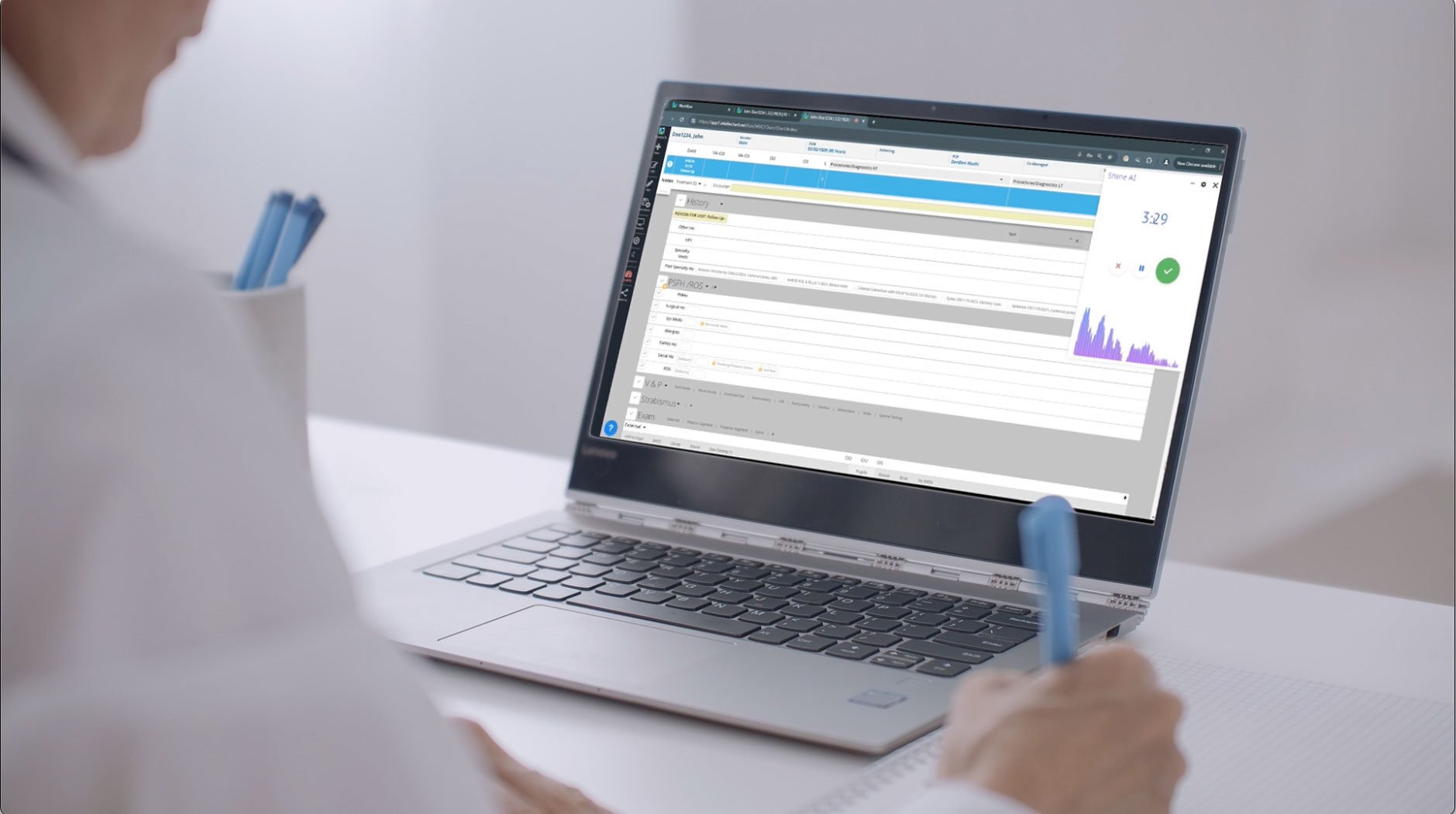
Nextech makes this simple by including a session with a MIPS Compliance Consultant in every new practice implementation. This session covers the eCQMs supported by Nextech and sets up the system for MIPS reporting.
The session also demonstrates the built-in Quality Assistance Tool, which provides visual cues, clear explanations, and live feedback on whether a measure was passed or failed — all without leaving the patient chart.
An EHR that is specialty specific and user friendly can make it easier for staff to enter the right information in the right places. Nextech offers EHRs specific to dermatology, ophthalmology, plastic surgery, med spa, and orthopedics, with a simple, easy-to-use interface.
Avoid Mistakes When Setting Up Reports
The most common mistake practices make when reporting eCQMs is not following the documentation that ensures a measure is completed.
An eCQM report looks for specific coding that tells the system that this patient has satisfied the numerator requirements for this measure.
If the practice is not using or documenting findings with that code, the patient’s outcomes won’t make it onto the report.
Other common setup mistakes include not updating the TIN for the current reporting year and not setting up the report to include all providers and locations.
The Role of Your EHR in Collecting eCQMs
A robust, up-to-date EHR is crucial for reporting eCQMs.
You must be using an EHR that meets CMS standards for interoperability, and it must be set up with a specific workflow to correctly tag and classify quality measure data.
Once eCQM collection is set up on the front end, the system automatically collects relevant data as it’s recorded in the EHR.
There is no manual chart abstraction, data entry, or data correction, and no manual submission of reports.
Nextech’s CMS-certified EHR is designed to make quality reporting as easy as possible. The user-friendly interface, comprehensive training, and outstanding customer support help practice staff use the system with confidence.
AI and automation tools can also make your EHR work smarter. For example, Nextech can save the quality measures each individual provider reports on in their provider settings. The Assisted Compliance Tool tracks and aggregates relevant compliance data for each patient visit.
eCQM FAQs
What are the benefits of eCQMs?
The key benefits of eCQMs are ease and efficiency. Because the data is automatically extracted from electronic health records, practice staff doesn’t have to manually extract, compile, and submit quality data.
Where does eCQM data come from?
The data reported in eCQMs flows directly from an EHR into a QRDA III file. To use eCQMs, a practice needs an advanced, certified EHR set up with an eCQM workflow.
What’s the difference between eCQMs and MIPS CQMs?
eCQMs and MIPS CQMs are both quality measures that healthcare providers report to the government.
The key difference is that eCQMs are electronically extracted from the provider’s EHR. MIPS CQMs can be extracted electronically or manually, and can come from any valid healthcare record: an EHR, an electronic registry, even a paper chart.
Heather Miller has more than 25 years of leadership experience in healthcare operational management, providing comprehensive medical consultation to hundreds of practices. Her expertise includes oversight of revenue cycle management, Medicaid and Medicare compliance, and workflow analysis to increase practice productivity. She has a proven track record in supporting clients in the adoption of electronic health records and providing strategy plans for annual MIPS reporting.
Heather holds a master’s degree in business administration from Rollins College - Crummer School of Business and a second master’s degree in Early Childhood Special Education from the University of Miami. She completed her undergraduate degree at the University of Tennessee in Special Education.
HERE ARE SOME RELATED ARTICLES YOU MAY FIND INTERESTING
MedSpa | Aesthetics | med spa
Gen Z Isn’t ‘Breaking’ the Med Spa Market. They’re Rewriting the Rules.
By: Robin Ntoh | February 11th, 2026