

Some say EMR. Some say EHR. Is this a “po-tay-to, po-tah-to” situation, or is there really a difference?
There are, in fact, significant differences between electronic medical records (EMR) and electronic health records (EHR).
Key Differences Between EMR and EHR
Both EMRs and EHRs are electronic records used by medical providers. But that’s where their similarity ends.
EHRs are a collaborative, portable record that gives any provider instant access to a patient’s complete health history. EMRs are internal records of a patient’s history at a single practice.
Here’s a breakdown of the key ways EMRs differ from EHRs.
|
What’s an EMR? |
What’s an EHR? |
|
A digital version of a patient chart |
A digital record of patient health information across providers |
|
Single-practice use; not easily shared with outside providers |
Allows providers in different practices and locations to collaborate in real time |
|
Cannot be updated by outside providers |
Follows the patient to new practices and providers |
|
For provider use; not intended for patient access and engagement |
Facilitates patient access and engagement |
What Is an EMR?
An EMR is a digital version of a paper chart. It helps a provider electronically track the diagnoses and treatments prescribed to a patient within that provider’s practice.
Compared to paper charting, EMRs are a vast improvement. They simplify data management, making it easy to track changes to a patient’s health over time.
A practice can use an electronic system to monitor and improve its overall quality of care. And the system can notify clinicians or their scheduling staff when a patient is due for a checkup or screening.
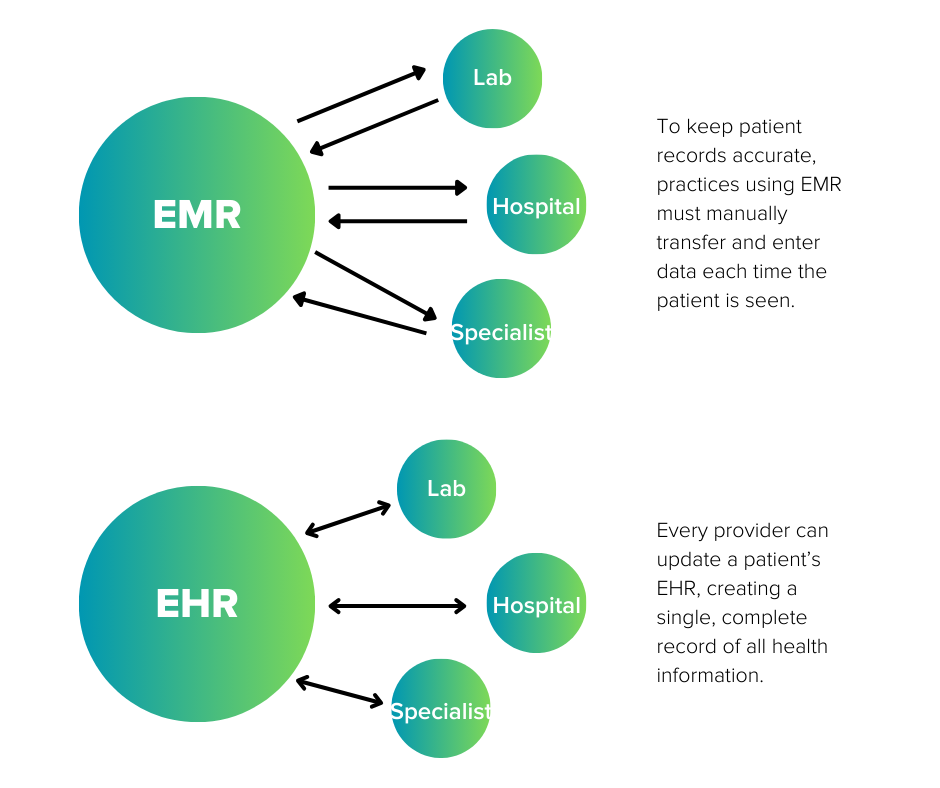
The biggest drawback to EMRs is their isolation. Sharing EMR information with an outside provider such as a hospital or specialist is difficult — it might even mean printing out the records to mail or fax them.
This separation cuts both ways. Not only can outside providers not access the patient history, they can’t update it.
For example, if an EMR-based dermatologist wants information about the skin treatment their patient received at a med spa, they have to request the documents and manually enter the information into their system.
To advise the med spa of the dermatologist’s treatment, the same process happens in reverse. This back-and-forth must happen every time for both practices to keep a complete record.
What Is an EHR?
An EHR is a complete digital picture of a patient’s health. It includes everything in an EMR, plus lab reports, imaging, diagnoses, and treatment plans from all the patient’s providers. Some even record wellness information from wearable devices like fitness trackers.
In the previous example, if the dermatologist and med spa were both using an EHR, each could instantly see what treatment was received at the other practice.
They could also access information the patient might not even realize is relevant — for example, if a primary care physician prescribed a medicine that causes photosensitivity.
When the patient moves to a new state, to a nursing home, or just to a provider across town, their electronic health record moves with them.
The EHR allows providers in different locations and different practices to collaborate on the patient’s health outcomes, sharing information in real time and creating a robust medical history.
Advantage of EHR over EMR
An EHR can be a powerful tool. The advantages of an EHR over an EMR include higher reimbursements, better patient outcomes, improved collaboration, portability, increased patient access and engagement, and data-based decision making.
Higher Reimbursements
The 21st Century Cures Act, enacted in 2019, made electronically shared health information the expected norm in American health care.
One of the key components of the federal law is the notion of interoperability. That means that electronic health information should be in a format that facilitates access, exchange, and use by all authorized medical providers.
Interoperability is so important to the federal government that medical practices not using a certified EHR face a 9% penalty on all Medicare Part B payments.
These practices are also automatically excluded from the MIPS promoting interoperability category, which makes up a quarter of the practice’s composite performance score.
Better Patient Outcomes
The more information a provider has about a patient, the more accurate their diagnosis will be. The interoperability of EHRs helps providers prescribe the most effective treatment and avoid negative interactions with other providers’ treatments.
In addition, many EHRs have information management tools for data analysis. These tools make it easier for providers to understand, interpret, and quickly respond to data.
This data can even be made anonymous and aggregated for research and care management applications. A practice could, for instance, track whether a specific diagnosis is on the rise in a certain population.
Improved Collaboration
EHRs are a secure platform providers can use to communicate with patients, staff, insurers, and other members of the care team.
Secure and real-time data exchange allows for meaningful collaboration on consultations and healthcare decisions. Portability and interoperability make for a quick, efficient referral process.
EHRs also reduce the risk of duplicate tests, as all providers have immediate access to lab results, radiology reports, and other diagnostic checks.

Portability
When a patient moves to a new area or adds a new provider to their care team, they don’t have to start their medical history from square one and hope they don’t forget anything. The big-picture view stored in the EHR follows them to every provider.
In the event a patient is incapacitated, an EHR allows responding providers to access critical information like chronic conditions, allergies, and medications, even if the patient can’t share the information themselves.
Patient Access and Engagement
HIPAA privacy rules put tight restrictions on who can access a patient’s medical history. But the 21st Century Cures Act is clear that patients should have easy access to their own records.
EHRs are compliant with both, protecting sensitive data from unauthorized access while allowing patients the information they need to proactively participate in their own healthcare.
EHRs often power patient portals, allowing patients to take an active role by viewing test results, scheduling appointments, and sending questions to their care team, even after hours.
Data-Based Decision Making
The benefits of the data in an EHR extend far beyond individual patients.
EHRs allow a practice to search and compile data for population health management and reporting.
An ophthalmologist near a wildfire area, for example, could analyze whether the changing air quality has a statistically significant impact on eye health.
The electronic system can also provide practice management data.
A growing demand for certain procedures might indicate a practice should train more staff or hire an additional provider. A growing number of patients from a specific ZIP code could lead a practice to expand its marketing efforts.
How to Choose an EHR for Your Practice in 4 Steps
- List your requirements. Before you start shopping, know what you need. Put together a selection committee representing every department in your practice. Whatever system you choose, you want to be sure it’s able to do everything your practice needs it to do, so give every department and role a chance to weigh in.
- Look for a specialist. There are EHRs targeted to every medical specialty. There are also general EHRs intended for broad application. Thanks to interoperability, all of these systems can talk to one another. So for the best out-of-the-box functionality, look for an EHR designed for your specialty. It’s going to have more of the features you want built in by default.
- Research vendors. When choosing a vendor, look at more than just the software features. Companies that involve clinical staff in their software’s development are more likely to nail the nuances that make the software user-friendly in a clinical environment. Also inquire about ongoing training and the availability of customer support.
- Request demos. Make a short list of vendors who meet all or most of the criteria you set. The final step is to view a demo of their product and see if you can imagine using it in your practice. Ask a lot of questions to find the product that’s the best fit.
Nextech offers industry-leading EHR solutions for dermatology, med spa, ophthalmology, and plastic surgery. Practices using Nextech see an average of 10% more patients per day, while reducing or eliminating after-hours charting.
Our software was developed by people with actual clinical and life sciences experience, and our chief medical officer is a practicing physician. Members of our customer service team also have clinical experience, so they can understand immediately where an issue stems from and how they can help.
To see if Nextech is the right fit for your practice, schedule a demo.
FAQs about EMR vs EHR
What are the disadvantages of EMR?
EMRs are better than paper charting, but they are at a steep disadvantage against the more powerful EHR.
- Practices using an EMR instead of an EHR are not eligible for full Medicare/Medicaid reimbursement.
- EMR is difficult to share with providers outside a single practice.
- When a patient sees multiple providers, there’s a heavy administrative burden on staff at each facility to maintain up-to-date records.
- EMR does not facilitate patient access and engagement.
- EMR does not provide big-picture data for population health and data-based business decisions.
Are EMRs HIPAA compliant?
Yes, reputable EMR and EHR systems both have privacy and security protocols to ensure HIPAA compliance.
How long does it take to learn to use an EHR?
Like all software, the learning curve varies based on an individual’s comfort with technology. Most practice teams spend about one week training in Nextech’s EHR and are comfortable using the system within a few weeks.
Does EHR make patients safer?
EHRs can contribute to patient safety. They allow every provider to see the patient’s entire medical record, including prescriptions, allergies, chronic conditions, and past diagnoses.
Can EMRs be used nationally?
No. EMRs cannot be used outside the practice that keeps them.
Is there free EHR software?
Yes and no. You might find vendors offering what they say is a “free” EMR/EHR solution. But every business needs to make money.
If they don’t charge for the software, they’re making their money another way — by delivering ads, charging for “add-ons” required to make the tool functional, or scraping and selling physician and patient data, for example.
Before you download a “free” EHR, read this so you know what you’re getting into.
About the author
Ryan Montalvo is a Senior Solutions Engineer at Nextech. Previously, he was an EHR Implementation Specialist, helping practices navigate the transition from paper to electronic records. He began his career as an ophthalmic scribe and is deeply familiar with the challenges of efficient medical charting.
HERE ARE SOME RELATED ARTICLES YOU MAY FIND INTERESTING
Revenue Cycle Management | Healthcare Technology
Setting the Revenue Cycle for Success
By: Nio Queiro | August 29th, 2024
How Healthcare Chatbots Help Clinics Provide Better Care
By: Nextech | May 31st, 2024