Latest Articles
The latest news and information regarding electronic medical records, practice management software, HIPAA, and security from Nextech.

By:
Nextech
November 19th, 2014
ICD stands for International Classification of Diseases. This international standard is used to document all different types of diseases and other health-related conditions in many official medical records. Most member states of the World Health Organization (WHO) started using ICD-10 (the most up-to-date version) since 1994. The United States is one of the few WHO members that still uses ICD-9 and has not yet transitioned to ICD-10.

Security & Data Management | Healthcare Technology
By:
Nextech
November 17th, 2014
Has a virus ever hit your computer networks or EMR software? How about a hard-drive failure, data leak, or someone with unauthorized access to your software (i.e. a hacker)? If you have experienced one or more of these IT issues, then you’re probably no stranger to the disastrous consequences it can have for your practice.

Regulatory & Compliance | Healthcare Technology
By:
Nextech
November 10th, 2014
For specialty practices large and small, optimizing functionality is a common concern, especially when taking into account future changes beyond Meaningful Use, the transition to ICD-10, and other heathcare mandates.

Regulatory & Compliance | Healthcare Technology
By:
Nextech
November 7th, 2014
The most recent delay in the ICD-10 transition was due, in part, to issues with vendor readiness. Another delay is extremely unlikely, yet readiness remains a potential issue with some suppliers. In fact, a recent survey from The Workgroup for Electronic Data Interchange (WEDI) revealed that only 40 percent of healthcare providers have “complete” solutions for ICD-10, an improvement of just 15 points compared to 12 months earlier, despite the extra development time. Specialty practices that rely on the remaining 60 percent of vendors whose solutions are not complete for ICD-10 should consider two key questions: How can I gauge whether my vendor will be ready in time? What represents sufficiently “complete” vendor software and services?

Healthcare Technology | Staff Management
By:
Nextech
October 28th, 2014
As specialty practices become increasingly reliant on information technology, effective “onboarding”—systems training for new hires—is essential to productivity. Unless a new hire has used exactly the same set-up previously, there is an important learning process for each system to be used, whether electronic medical record (EMR), practice management, revenue management or patient engagement. Think about how much everyone in the practice had to learn at initial implementation; each new hire must go through that same process—without the benefit of group learning. Here are six best practices that will improve both the speed and effectiveness of onboarding: Assess the new hire’s computer skills during the hiring process. Don’t assume that everyone needs training only in specific systems. If a new hire worked previously at a primarily paper-based practice, determine whether you need to line up supplemental computer training or have other additional resources available as the start date approaches. Prepare for training in advance of the new hire’s arrival. To ensure that all helpful materials are available from day one, assemble vendor training materials and identify vendor resources appropriate for the new hire’s job function ahead of time. Practices should look for a vendor that provides unique training for each specific job function, ensuring new employees are able to leverage the system in a way that meets their unique workflow needs. Encourage peer-to-peer training. Nobody wants to begin work by pouring through training materials. One-on-one, real-time training from proficient users who perform the same function invites question-and-answer skill building and quicker mastery of specialty and practice specifics. Focus strictly on the new hire’s function. Very few people within any specialty practice need to use every feature of an EMR, for example. Plan onboarding around what the new hire must master to succeed in the assigned role. Set realistic expectations and communicate them clearly. As was the case with initial system implementations, not everyone learns at the same rate. Give a clear indication of the time expected for learning, and invite the new hire to ask for help when specific areas prove challenging.

Healthcare Technology | Events
By:
Nextech
October 3rd, 2014
Going to a user conference, attendees can predict that they will hear from a multitude of company appointed speakers as well as industry thought leaders. The knowledge gained is valuable and expected for someone looking to get a better understanding of the product they are using. Although this aspect of attending a software user conference is of paramount importance, another component not to be minimalized is the opportunity to get insights from fellow EMR and practice management users to help improve your own usability.

Regulatory & Compliance | Healthcare Technology
By:
Nextech
October 2nd, 2014
While most discussion of the October 1, 2015, transition to ICD-10 focuses on the billing function, ICD-10’s impact will extend significantly to the clinical side of practices as well. Documentation captured in electronic medical records (EMRs) must give coders information that supports the new coding standard if claims are to be accurate and complete. Fortunately, providers have less learning ahead than coders do. And unlike coders, they don’t have to wait until the transition date to begin actually performing in ICD-10 terms. They can, and should, start soon. Clinicians who are not yet familiar with the impact of ICD-10 on their function can read a two-page summary titled “Effects on Clinical Documentation” in the CMS ICD-10 Implementation Guide for Small and Medium Practices. In addition, each practice will want to form a game plan for readying clinicians for the effect the transition will have on its particular specialty.

Patient Engagement | Healthcare Technology
By:
Nextech
September 24th, 2014
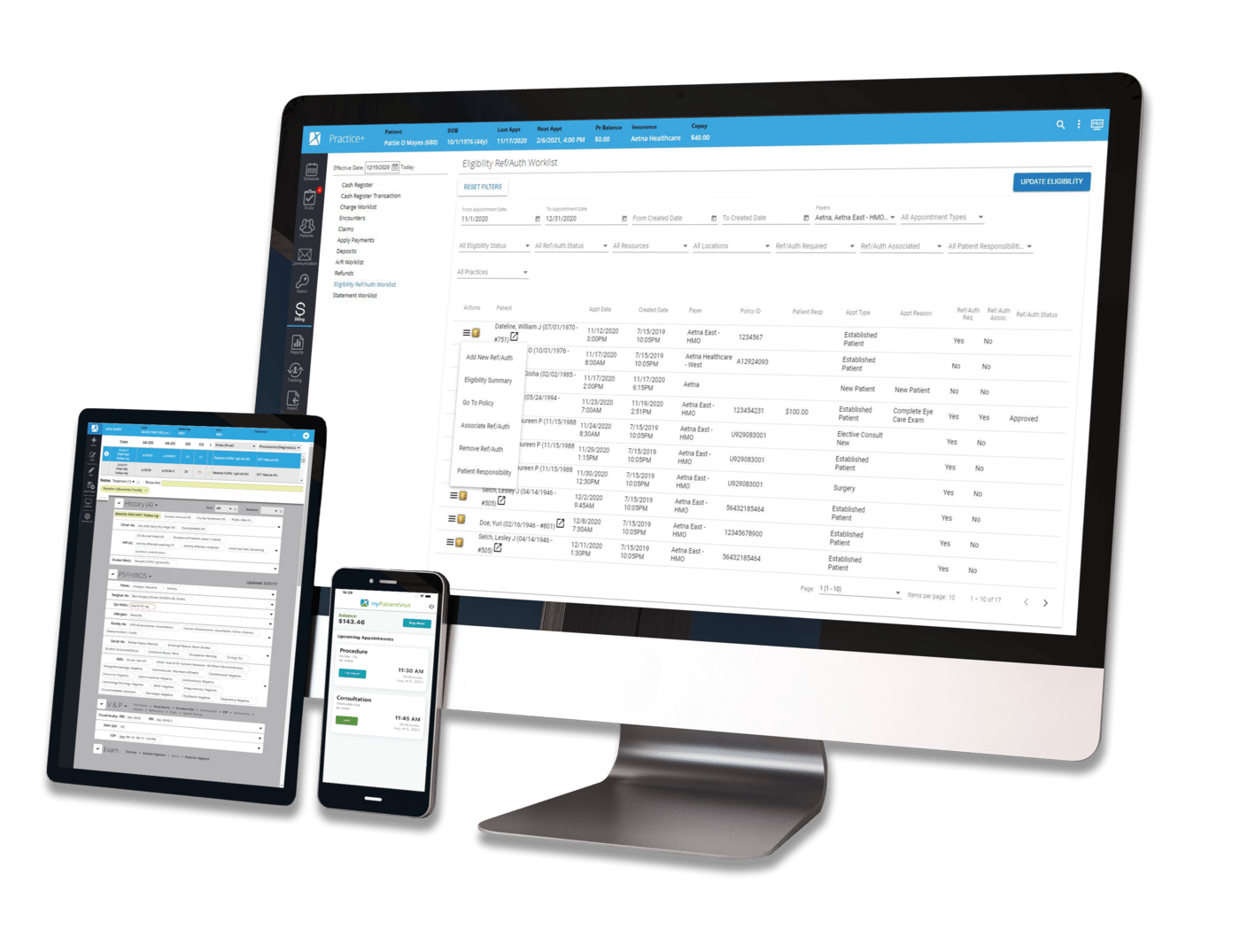
Physicians increasingly expect the ability to access EMRs on their mobile devices. As we relayed in this space in July, a recent survey found that 100 percent of physician practices that are considering switching EMRs view mobile access as a requirement for their next system.