The Physician Quality Reporting System is gaining momentum as we move forward into 2016. With new acronyms (MIPS, MACRA, PQRS, MU, VBM, etc.) making an appearance on what feels like a monthly basis, it’s important to know where the program is headed and what your game plan will be for avoiding penalties.
The Introduction of MIPS
The Merit Based Incentive Payment System, or MIPS, is a continuation of all of the existing programs, including PQRS, Meaningful Use, and the Value Based Payment Modifier (VBM). The core of this system is promoting value over volume and paying providers based on the quality of the care they are providing, versus the standard fee schedules that will become a thing of the past by the year 2020. More specifically, MIPS is looking at quality, resource use, clinical practice improvement activities, and meaningful use of your certified EHR technology.
Something important to know about all of these programs, as they continue to meld in the future, is that their penalties will add up to an alarming percentage of your Medicare Part B payments if you fail to meet the minimum reporting requirements.
Reporting in 2016
For 2016 PQRS reporting, you need to report nine measures across three domains and the reporting period is the entire calendar year. These requirements are unchanged from 2015. The difference for Nextech users in the Dermatology and Ophthalmology specialties is that there are new integrated options that will make reporting in 2016 as seamless as it gets. These seamless options come in the form of Clinical Registries, such as IRIS or DataDerm, all powered by FigMD.
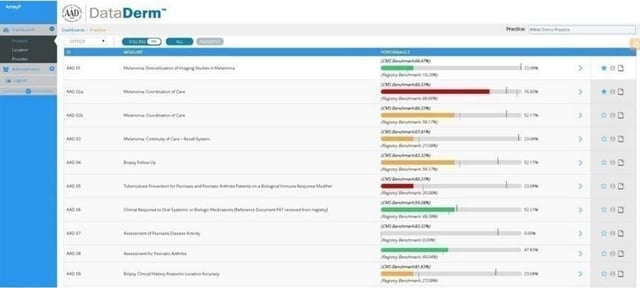
If you choose the Clinical Registry for your PQRS reporting method in 2016, the registry will have read-only access to your database, and they will collect and submit the data on your behalf. The initial process includes the registry contacting your practice as well as setting up connection (via a connection request form that will be sent to Nextech). Nextech will provide the registry with the access they need. Then, the registry will work with the practice on mapping. Once the mapping is completed, there will be continuous reporting. Throughout the year, you can log into the registry website and navigate the easy to use dashboard to see how you’re performing compared to national benchmarks for each objective (see below DataDerm dashboard example).
For an easy to use beginner guide for reporting with Clinical Registries in 2016, click here!
Important Deadlines
For Dermatology Practices that choose to report through DataDerm in 2016:
- July 1, 2016 – Last day for EHR-based practices to enroll in DataDerm for 2016 PQRS reporting (If you’ve already registered with DataDerm to help take care of your Meaningful Use Public Health Reporting, then you won’t need to register again)
- December 16, 2016 – Last day to purchase PQRS submission option for those enrolled (DataDerm is the American Academy of Dermatology’s only registry option this year)
- January 13, 2017 – Deadline for reporting 2016 PQRS data for the 2016 reporting period (Jan 1 – Dec 31, 2016)
For Ophthalmology Practices that choose to report through IRIS in 2016:
- June 1, 2016 – Submit signed agreements
- August 1, 2016 – Ensure your EHR system is mapped to the IRIS Registry
- January 15, 2017 – Submit your data-release consent form (this form allows the registry to submit your data to CMS)
The Direct EHR Reporting Method Through Nextech
In 2015, Nextech introduced the option of Direct EHR reporting for PQRS. In 2016, this is still a valid and simple option for Nextech users, particularly our Plastic Surgery Practices that do not have a PQRS registry option. Just like last year, you can align your Clinical Quality Measures for the Meaningful Use EHR Incentive program with the nine PQRS measures across three domains. The benefit to this option is that there are no threshold requirements for each objective, as there would be if you reported through a registry or through your claims. The bare minimum requirements are that you have nine measures, all with a denominator, and at least one measure that has a performance rate greater than 0%. For more information on this option, please see this user guide provided my CMS: Direct EHR Reporting Made Simple.
Nextech recommends the following measures for Plastic Surgery offices reporting through the Direct EHR Reporting Method:
- CMS156 Use of High Risk Medications in the Elderly
- CMS68 Documentation of Current Medications in the Medical Record
- CMS50 Closing the Referral loop: Receipt of Specialist Report
- CMS138 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
- CMS147 Preventive Care and Screening: Influenza Immunization
- CMS69 Preventive Care and Screening: Body Mass Index (BMI) Screening and Follow up
- CMS125 Breast Cancer Screening
- CMS130 Colorectal Cancer Screening
- CMS165 Controlling High Blood Pressure
Action Step for the Direct EHR Reporting Method
If you did not report this way in 2015, you will want to make sure you register with the CMS Enterprise Portal. The registration process is lengthy and sometimes takes troubleshooting with the Quality Net Helpdesk, so it is important to get this done early! Once you have registered, when it comes time to submit between January 1st and February 28th 2017, you would submit the QRDAIII file, generated in Nextech, to the Quality Net Portal. For quick reference guides for this website, click here.
Have a Game Plan
Whether you submit through a Qualified Clinical Data Registry, the Direct EHR reporting method, claims, etc., the important thing is that you are reporting and avoiding the mounting penalties. CMS has already released news that other major commercial and private health plans have agreed to work towards aligning measures, adding more meaningful measures, and reducing extra efforts. This does not change the penalties, as they still come from Medicare right now, but who knows how that will change.
HERE ARE SOME RELATED ARTICLES YOU MAY FIND INTERESTING
Regulatory & Compliance | Revenue & Finances
What Is PECOS? Step-by-Step Guidance for Specialty Practice Owners
By: Nextech | January 5th, 2026
MedSpa | Regulatory & Compliance | Aesthetics
IV Therapy Laws by State
By: Nextech | April 10th, 2025
MedSpa | Regulatory & Compliance | Aesthetics | podcast
The Current & Future State of the Medical Spa Business with Alex Thiersch
By: Tyler Terry | April 24th, 2024

